Colposcopy: What to Expect
A colposcopy is a test to take a closer look at your cervix. If your cervical screening (smear test) has shown some cell changes, a colposcopy can help determine the extent of these changes and whether you need treatment. Understanding what this procedure involves can help ease anxiety and prepare you for what to expect.
What is a colposcopy?
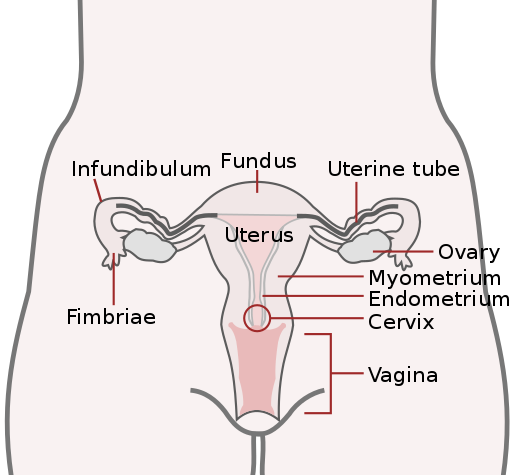
A colposcopy is a detailed examination of the cervix (the opening to your womb from your vagina) using a special microscope called a colposcope. The colposcope stays outside your body and provides a magnified view of the cervix, allowing the doctor to examine any abnormal areas in detail.
The procedure is usually performed by a specially trained doctor or nurse and typically takes about 15-20 minutes. It's usually done in an outpatient clinic, which means you won't need to stay overnight in hospital.
A colposcopy is often done if cervical screening finds changes to your cells that are caused by certain types of human papillomavirus (HPV). These changed cells can sometimes develop into cervical cancer if left untreated. The colposcopy allows healthcare professionals to assess these changes and decide if treatment is needed.
Why it's done
A colposcopy may be recommended for several reasons:
- You've had an abnormal cervical screening result showing cell changes (dyskaryosis)
- You've tested positive for high-risk human papillomavirus (HPV)
- Your cervix looks unusual during a routine examination
- You've had bleeding after sex or between periods that requires investigation
- To monitor previously identified cell changes
- To check the effectiveness of treatment for cervical abnormalities
It's important to remember that an abnormal screening result doesn't mean you have cancer. In fact, most women who have a colposcopy don't have cancer. The procedure is primarily a preventative measure to identify any pre-cancerous changes that can be treated before they develop into cancer.
Understanding HPV: Human papillomavirus (HPV) is a common virus that most people will have at some point in their lives. There are many types of HPV, and most are harmless. However, some high-risk types can cause cell changes that may lead to cancer if left untreated. HPV infection is the main cause of cervical cancer, but it usually takes many years for cancer to develop after HPV infection.
Getting ready
Preparing for a colposcopy involves a few simple steps:
- Try to schedule your appointment when you're not having your period, as blood can make it difficult to get a clear view of your cervix
- Avoid using vaginal medications, creams, or lubricants for at least 24 hours before your appointment
- Avoid sexual intercourse for 24-48 hours before the procedure
- You may wish to take a mild pain reliever about an hour before your appointment to reduce any discomfort
- Wear comfortable, loose-fitting clothes to your appointment
- You don't need to fast before a colposcopy; eating and drinking normally is fine
- If you're pregnant or think you might be, inform your healthcare provider before the procedure
It's also helpful to bring someone with you to the appointment for support, especially if you're feeling anxious. Some women find it reassuring to have a friend or partner with them, though this is entirely your choice.
What happens on the day
Understanding what happens during a colposcopy can help reduce anxiety about the procedure:
- You'll be asked to undress from the waist down (a gown or sheet will be provided for privacy) and lie on an examination table with your feet in supports, similar to having a cervical screening
- A smooth, tube-shaped tool (a speculum) is gently placed into your vagina to hold it open so the cervix can be seen clearly
- The colposcope (which looks like a pair of binoculars on a stand) is positioned outside your body, about 30 cm from your vulva, giving the doctor a magnified view of your cervix
- The doctor will apply a solution to your cervix using a cotton swab - this may feel slightly cold or tingling but is not painful. This solution helps highlight any abnormal areas
- If abnormal areas are identified, a small sample of tissue (biopsy) may be taken for further testing. This involves removing a tiny piece of tissue (about the size of a pinhead) from the cervix
- Taking a biopsy may cause mild cramping or pinching sensations, and some women experience brief discomfort similar to menstrual cramps
- If larger areas of abnormal cells are found, treatment might be recommended right away or at a later appointment
The entire procedure typically takes 15-20 minutes. Some women experience mild discomfort during a colposcopy, similar to period cramps, while others report little or no discomfort. If you feel pain or significant discomfort during the procedure, let your doctor know right away.
Treatment during colposcopy: Sometimes, if the abnormal area is small and clearly defined, your doctor might suggest treating it during the same appointment. This is known as "see and treat" approach. The most common treatment is LLETZ (Large Loop Excision of the Transformation Zone), which uses a thin wire loop with an electrical current to remove the abnormal cells. Your doctor will discuss whether this is appropriate for you and explain the procedure fully before proceeding.
Results
What happens after your colposcopy depends on the findings:
- If no abnormal cells are found, you may simply be advised to return to routine cervical screening
- If a biopsy was taken, you'll usually get the results within 2-4 weeks
- Your results will typically be classified as:
- Normal - no abnormal cells found
- CIN 1 - mild changes that often clear up on their own without treatment
- CIN 2 or CIN 3 - moderate to severe changes that usually require treatment
- CGIN - abnormal glandular cells that usually require treatment
- If treatment is needed, this might be done during a future appointment or, in some cases, may have been done during your colposcopy
- After treatment, you'll need follow-up appointments to ensure the abnormal cells have been completely removed
It's important to remember that even if abnormal cells are found, this doesn't mean you have cancer. CIN (Cervical Intraepithelial Neoplasia) describes abnormal changes in the cells of the cervix that, if left untreated, could potentially develop into cervical cancer over time. Treatment at this pre-cancerous stage is very effective.
After your colposcopy
After your colposcopy, you should be able to resume most normal activities right away, but there are a few things to keep in mind:
- If you had a biopsy, you may experience mild cramping or spotting for a day or two
- You may notice a dark discharge for a few days, which is normal and is due to the solution used during the procedure
- Avoid using tampons, having sex, or swimming for at least a week if you had a biopsy or treatment
- Take over-the-counter pain relievers if you experience discomfort
- Contact your healthcare provider if you experience heavy bleeding (heavier than a period), severe pain, fever, or foul-smelling discharge
Final Thoughts
A colposcopy is a valuable diagnostic tool that helps detect and prevent cervical cancer by identifying abnormal cells at an early stage when treatment is most effective. While the procedure might cause some anxiety, understanding what to expect can help you feel more prepared and comfortable.
Remember that having a colposcopy does not mean you have cancer - it's primarily a preventative measure. The vast majority of women who undergo colposcopy and any subsequent treatment go on to have normal cervical screening results in the future.
If you have any concerns or questions about your colposcopy, don't hesitate to discuss these with your healthcare provider. They can provide you with personalized information and support throughout the process.
