Complete Guide to Cervical Cerclage
Cervical cerclage, also known as a cervical stitch, is a procedure that can help prevent premature birth or late miscarriage in certain pregnancies. While not every expectant mother will need this intervention, understanding what cervical cerclage involves can be valuable information for those at risk of preterm birth. This guide explains when cervical cerclage is needed, how the procedure is performed, and what to expect during recovery.
What is Cervical Cerclage?
Cervical cerclage is an operation where a stitch is placed around your cervix (the neck of your womb) like a purse string, in order to try to keep it closed. The procedure aims to provide additional support to the cervix when there is concern that it might shorten or open too early during pregnancy, which could lead to miscarriage or premature birth.
The stitch is typically placed between 12 and 24 weeks of pregnancy as a planned procedure, although in some cases it may be done at later stages or even before pregnancy.
Types of Cervical Cerclage
There are several types of cervical cerclage procedures:
- Transvaginal Cerclage (TVC): The most common approach, where the stitch is placed through the vagina
- Transabdominal Cerclage (TAC): A less common procedure where the stitch is placed through an abdominal incision
- Emergency Cerclage: Performed after the cervix has already started to open
Your healthcare provider will recommend the most appropriate type based on your specific circumstances and medical history.
When is Cervical Cerclage Needed?
You may be considered for a cervical cerclage if you have risk factors for premature birth related to cervical issues. Your healthcare professional might recommend it if:
- You have had a miscarriage after 16 weeks of pregnancy
- You have had a previous birth before 34 weeks of pregnancy
- Your waters broke before 34 weeks in a previous pregnancy
- You have had certain types of treatment to your cervix (such as LLETZ or cone biopsy for abnormal smear treatment)
- You have scarring to your endometrium or your uterus is an unusual shape
- You have had a previous caesarean birth when you were fully dilated
- You have needed a cervical stitch in previous pregnancies
If you're at increased risk of preterm birth, your healthcare team may arrange for you to have transvaginal ultrasound scans to measure your cervix. A cervical length of less than 25 mm may indicate the need for intervention.
Individual Assessment: The decision to perform cervical cerclage is always based on your individual circumstances. Not everyone with these risk factors will need a cerclage, and your healthcare team will discuss the potential benefits and risks with you before making a recommendation.
When Cervical Cerclage May Not Be Advised
There are situations where cervical cerclage may not be recommended as it could carry risks without improving outcomes. These include:
- If you have any signs of infection
- If you are experiencing vaginal bleeding
- If you are having contractions
- If your waters have already broken
For multiple pregnancies (twins or more), there is limited evidence that cerclage prevents early labour, and your care will be tailored to your specific situation.
Preparing for Cervical Cerclage
If you're scheduled for a cervical cerclage, your healthcare team will provide specific instructions, but generally you can expect:
- A consultation to discuss the procedure, including risks and benefits
- Pre-procedure tests, which may include blood tests and ultrasound scans
- Instructions about fasting before the procedure (typically no food for 6-8 hours)
- Guidance on which medications to take or avoid before the procedure
- Information about the type of anesthesia that will be used
It's important to discuss any concerns or questions you have with your healthcare provider before the day of the procedure.
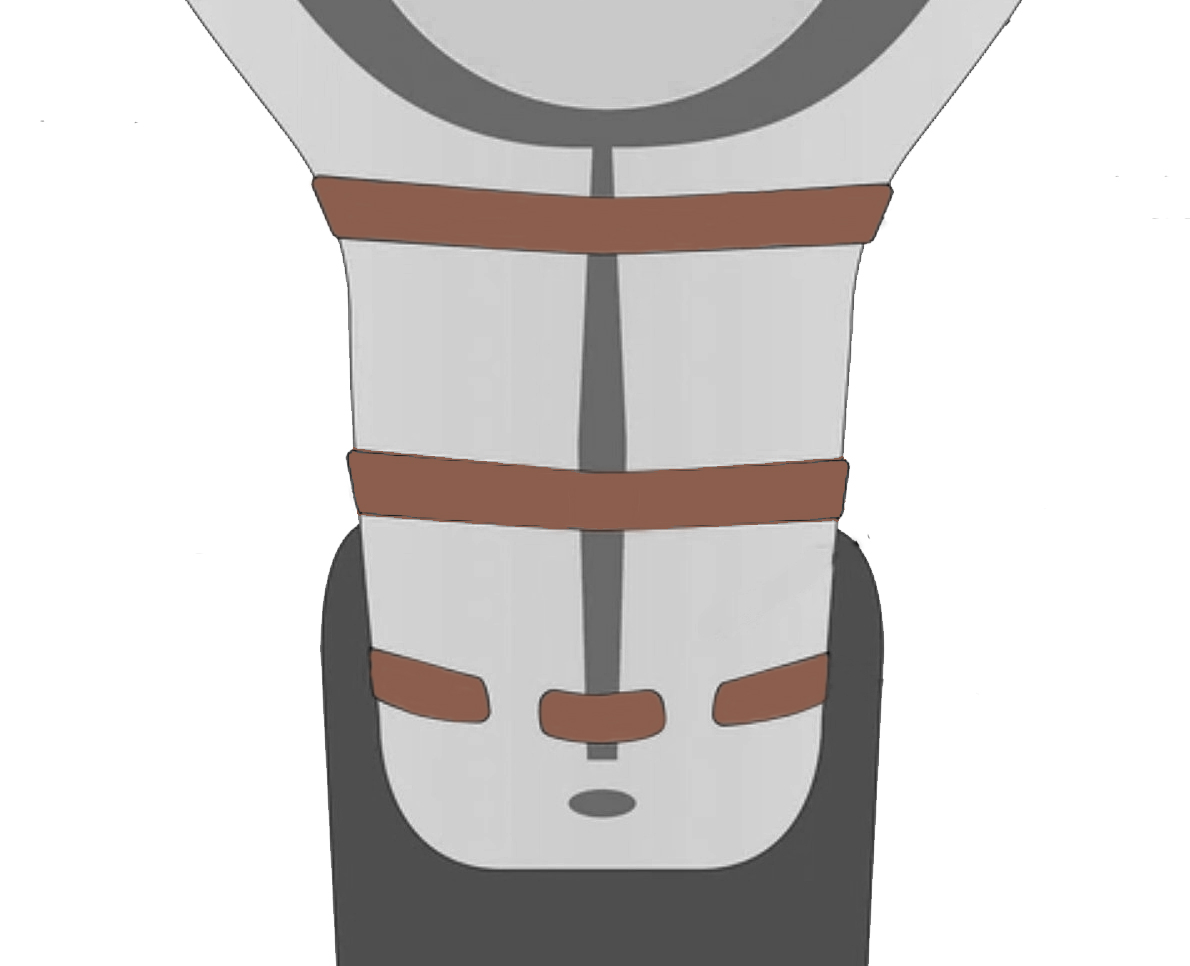
How is Transvaginal Cerclage Performed?
The transvaginal cerclage procedure takes place in an operating theatre and typically follows these steps:
- You will receive either a spinal anesthetic (where you remain awake but numb from the waist down) or a general anesthetic (where you will be asleep)
- Your legs will be positioned in supports and sterile covers will be used
- The surgeon will insert a speculum into your vagina to access the cervix
- The stitch is placed around the cervix like a purse string and then tightened and tied
- The entire operation typically takes less than one hour
- You may have a catheter inserted into your bladder that will be removed once the anesthetic wears off
You will likely be offered antibiotics during the operation and medication to ease any discomfort afterward. Most women can go home the same day, though some may be advised to stay in hospital longer depending on their circumstances.
Transabdominal Cerclage (TAC)
This less common procedure involves placing a stitch around the cervix through an abdominal approach. It may be recommended if:
- Previous vaginal cerclage attempts have failed
- It is not possible to insert a vaginal stitch due to anatomical reasons
A TAC can be performed either before pregnancy or in early pregnancy. The procedure may be done through a small abdominal incision (through which a Caesarean section can be performed later). This type of stitch remains in place permanently, and any future babies would need to be delivered by Caesarean section.
Emergency Cerclage
In some cases, you may be offered a cervical stitch as an emergency procedure after your cervix has already started to open. This is done to help prevent late miscarriage or early preterm birth.
Emergency cerclage carries higher risks and is less likely to be successful compared to planned procedures. Your healthcare team will discuss the specific risks and potential benefits in your situation.
Potential Risks of Cervical Cerclage
Like any surgical procedure, cervical cerclage carries certain risks, including:
- Bleeding
- Injury to the bladder
- Injury to the cervix
- Premature rupture of membranes (waters breaking early)
- Infection
It's important to note that even with successful placement, the stitch may not always prevent premature birth. If you go into labour with the stitch in place, there is a risk of cervical injury during labour.
A vaginal cervical stitch does not increase your chances of needing induction of labour or a caesarean section.
Recovery and Aftercare
After the cervical cerclage procedure:
- You may experience some vaginal bleeding or brownish discharge for a day or two
- You should not feel significant discomfort from the stitch itself
- Once recovered from the operation, you can usually carry on as normal for the rest of your pregnancy
- Bed rest is not routinely recommended
- You can resume sexual activity when you feel comfortable, though occasionally your partner may be able to feel the stitch
Warning Signs: Contact your healthcare team immediately if you experience any of the following after cerclage placement:
- Contractions or cramping abdominal pain
- Continued or heavy vaginal bleeding
- Your waters breaking
- Smelly or green vaginal discharge
Removal of the Cerclage
Your cervical stitch will typically be removed at around 36-37 weeks of pregnancy, unless you go into labour before then. The removal process:
- Takes place in hospital
- Involves inserting a speculum into your vagina
- The stitch is cut and removed
- Usually takes just a few minutes
- Normally does not require anesthesia, though options for pain relief can be discussed if you're concerned
You may notice some blood staining or vaginal spotting afterward, which should settle within 24 hours, though a brown discharge may last longer.
Most women do not go into labour immediately after stitch removal. If you have a planned caesarean, the stitch can be removed during that procedure.
Important: If you go into labour with the cervical stitch still in place, contact your maternity unit immediately. It's crucial to have the stitch removed to prevent damage to your cervix.
If your waters break early but you are not in labour, the stitch will usually be removed because of the increased risk of infection. The timing will depend on your individual situation.
Future Pregnancies
If you have had a cervical stitch in a previous pregnancy, you may be offered one again in future pregnancies. You should be referred to a specialist clinic early in your next pregnancy to discuss your care plan.
Your healthcare team will consider your previous pregnancy history and current circumstances to determine the best approach for any subsequent pregnancies.
Final Thoughts
Cervical cerclage is an important intervention that can help prevent premature birth in women at risk due to cervical issues. While the procedure carries some risks, for many women, these are outweighed by the potential benefits of prolonging pregnancy.
Every pregnancy is unique, and the decision to perform cerclage should be made after careful consideration of your individual circumstances. Open communication with your healthcare team is essential throughout this process. Don't hesitate to ask questions or express concerns about any aspect of the procedure or aftercare.
Remember that the goal of cervical cerclage is to support you in achieving a healthy, full-term pregnancy, and your healthcare providers are there to guide you through every step of the journey.
